Pharmacological and Parental Therapies / 04
Make sure to:
- Learn the main antidotes for the most common drug overdose scenarios.
- Identify the main signs that indicate an IV or catheter is misplaced or causing potential harm to the patient/client.
- Learn how to communicate with patients about the main side effects, identify adverse reactions, and know when to discontinue treatment and call the physician or visit the ER.
 An Adverse Reaction (AR) is an unwanted effect of a drug in the human body. Adverse reactions also play a role in patient's mobility and mortality, emphasizing the importance of patient education for drug safety. It is the nurse’s role to ensure the patient is aware of possible signs and symptoms of AR and the severity of each.
An Adverse Reaction (AR) is an unwanted effect of a drug in the human body. Adverse reactions also play a role in patient's mobility and mortality, emphasizing the importance of patient education for drug safety. It is the nurse’s role to ensure the patient is aware of possible signs and symptoms of AR and the severity of each.
Patient safety and treatment efficacy are the responsibility of all members of the healthcare team. Keep in mind, during this topic, the main key concepts: hepatotoxicity (damage to the liver caused by a drug) and adjustment to renal patients, whether they are on dialysis or not.
One of the main processes nurses perform in acute and ambulatory healthcare settings is IV therapy/solutions. Learn the key concepts about doing it properly and safely (Montané & Santesmases, 2020).
Drug safety and efficacy have been a concern in the healthcare industry for a long time. Clinical trials for drug testing incorporate many safety check procedures to ensure that the drug is safe and ready for patient delivery. The U.S. government has an official entity whose job is to establish vigilance and rules to guarantee the safety and efficacy of food and drugs sold to consumers, whether they are prescription or over-the-counter. Healthcare professionals can report any adverse reactions encountered during their daily practice (see additional resources to find out more about this program).
In the light of this very important subject, the key term: Pharmacovigilance will be introduced.
Adverse drug reaction (ADR) is defined by the World Health Organization (1972) as “a response to a drug which is noxious and unintended, occurring at doses normally used in humans for the prophylaxis, diagnosis, or disease therapy, or for the modification of physiological function.” Moreover, Pharmacovigilance (PV) refers to ADR, defined by the World Health Organization (1972) as “the science and activities related to the detection, assessment, understanding, and prevention of adverse effects or any other potential drug-related problems.”
The nurse’s role and attitude towards pharmacovigilance are to report ADR to the healthcare team in order to advocate for treatment efficacy and patient safety. In this Topic, the identification of some of the main ADR and the primary causes for drug overdose encountered in the acute and ambulatory healthcare settings will be reviewed.
3.1 How to Identify the Most Common Side Effects
 In clinical practice, the nurse will be able to identify the most common ADRs and their physical signs. The goal of the nursing process is to immediately report them to the physician and the healthcare team to avoid any life-threatening complications.
In clinical practice, the nurse will be able to identify the most common ADRs and their physical signs. The goal of the nursing process is to immediately report them to the physician and the healthcare team to avoid any life-threatening complications.
For NCLEX purposes, the most common side effects will be categorized by sign or symptom:
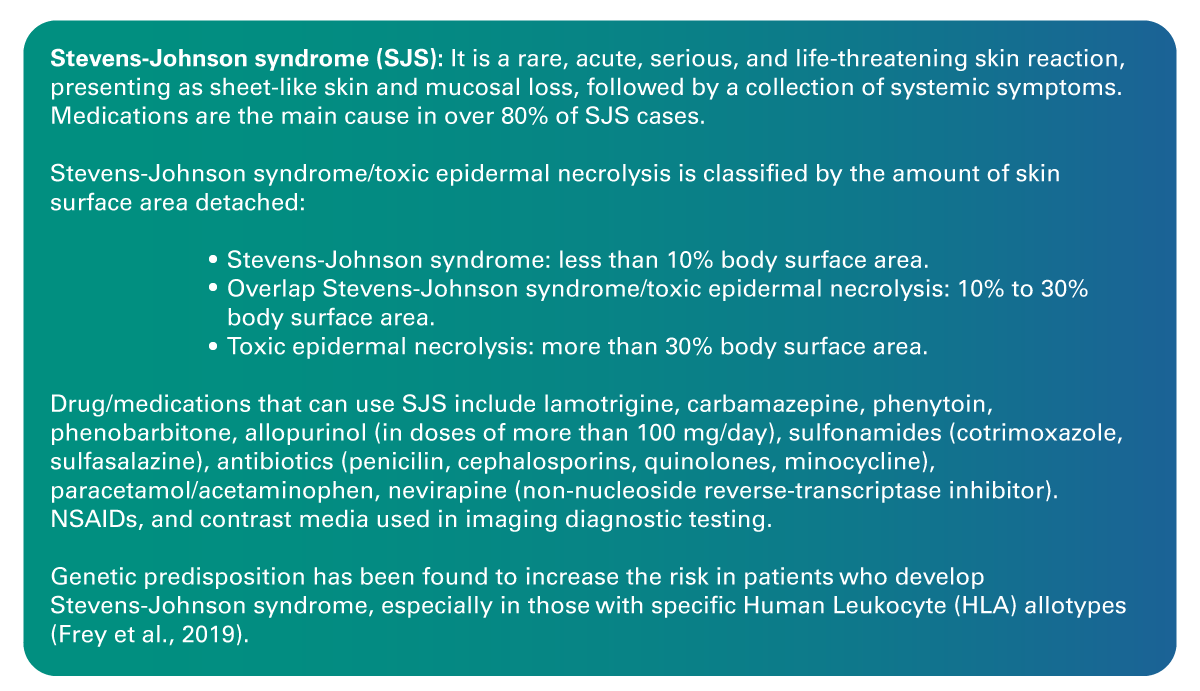
- Dermatitis: Probably one of the most visible ADRs, may also be considered a mild effect. However, some medications, especially antibiotics, in specific patients can cause a life-threatening condition that presents as dermatitis in the onset phase .
- Constipation: Is caused by many medications, including analgesics (codeine, morphine, and tramadol), antispasmodics, tricyclic antidepressants (amitriptyline), calcium channel blockers, other antihypertensive drugs, antipsychotics (clozapine, thioridazine, chlorpromazine), and diuretics. Constipation may not be a life-threatening situation; however, it is a very common side effect of many drug therapies, resulting in a frequent chief complaint and a source of discomfort for the patient. Notify the healthcare team as soon as it is presented to make dose or drug adjustments, along with other general care adjustments such as increasing water intake, making diet changes, and removing ambulation or bed-to-chair restrictions to increase GI motility.
- Diarrhea: Is associated with several medications, such as amoxicillin, cephalosporins, and clindamycin. Metformin is also among the medications whose most common side effect is diarrhea, with up to 63% of patients complaining of it. Antidepressants such as Zoloft, Prozac, and Lexapro, as well as beta blockers and ACE inhibitors, are also associated with diarrhea. Patients/clients with hypertension are at high risk of developing this side effect. Proton pump inhibitors, another popular over-the-counter medication, can cause diarrhea when taken chronically. Levothyroxine, a common treatment for hypothyroidism, has also been reported to cause diarrhea in up to 25% of users. Diarrhea is usually a self-limited ADR, meaning that once the cause is removed, bowel movements and consistency should return to normal. It is important to monitor for signs of dehydration, especially in pediatric and elderly patients.
- Arrhythmias
- Bleeding or increased PT and PTT times
- Neoplasia
- Suicidal ideation
Examples of more serious effects include:
Intravenous Therapy, Types of IV's and Common Side Effects
IV fluids are an essential part of the nursing process. Nurses administer IV fluids not only as a delivery mechanism for drugs but also to correct essential physiological processes, such as electrolyte imbalance and volume depletion. The physician will order the specific type of fluid based on the assessment of the patient's current condition. However, it is the nurse, a crucial member of the healthcare team, who oversees this duty (Ernstmeyer & Christman, 2021).
For nursing students and nurses, it is essential to be familiar with IV fluid types and fluid tonicity. Gain knowledge about the distinctions among isotonic solutions, hypertonic solutions, and hypotonic solutions (crystalloid solutions).
IV is the commonly used abbreviation for intravenous. When administering IV fluids, it is crucial to understand how they work and what to monitor in the patients.
Nurses administer IV fluids according to healthcare provider instructions to treat fluid volume deficits, such as dehydration, electrolyte imbalances, and other conditions.
The human body comprises two main compartments: the intracellular space and extracellular space. The intracellular space is found within the cell membrane while the extracellular compartment is located outside the cell membrane and consists of the interstitial compartment, intravascular compartment (plasma), and the transcellular compartment. Fluids can move into or out of each compartment through a well-known physiological process of osmosis (Ernstmeyer & Christman, 2021).
Types of IV Solutions
Isotonic: The osmolality is close to that of the extracellular fluid (ECF). This solution does not cause red blood cells to swell or shrink. It is commonly indicated in the presence of intravascular dehydration usually caused by activities like running, labor, fever or infection (Ernstmeyer & Christman, 2021).
- Normal saline (0.9% NS)
- Lactate Ringer's
- 5% dextrose in water
Hypotonic: The osmolality is lower than that in the ECF, causing fluid to move from the extracellular compartment to the intracellular compartment. It is indicated in the presence of cellular dehydration, especially in patients with extended periods of dehydration. It is also used in the management of volume-depleted patients/clients who are hyperosmolar (hypernatremia, hyperglycemia) (Ernstmeyer & Christman, 2021).
- Normal saline (0.5% NS)
- 2.5% dextrose in 0.45% saline (D2.5 45% NS)
Hypertonic: The osmolality is higher than the ECF, and it is indicated in the presence of intravascular dehydration with interstitial or cellular overhydration. Given the nature of this specific type of fluid, caution should be exercised. It can be indicated for caloric replacement or when serum osmolality is dangerously low. Examples include dehydration from surgery or blood loss causes (Ernstmeyer & Christman, 2021).
- 5% dextrose in lactated Ringer’s (D5LR)
- 5% dextrose in 0.45% saline (D5NS)
- 10% dextrose in water (D10W)
Figure 1
Isotonic, Hypotonic and Hypertonic Solutions Representation
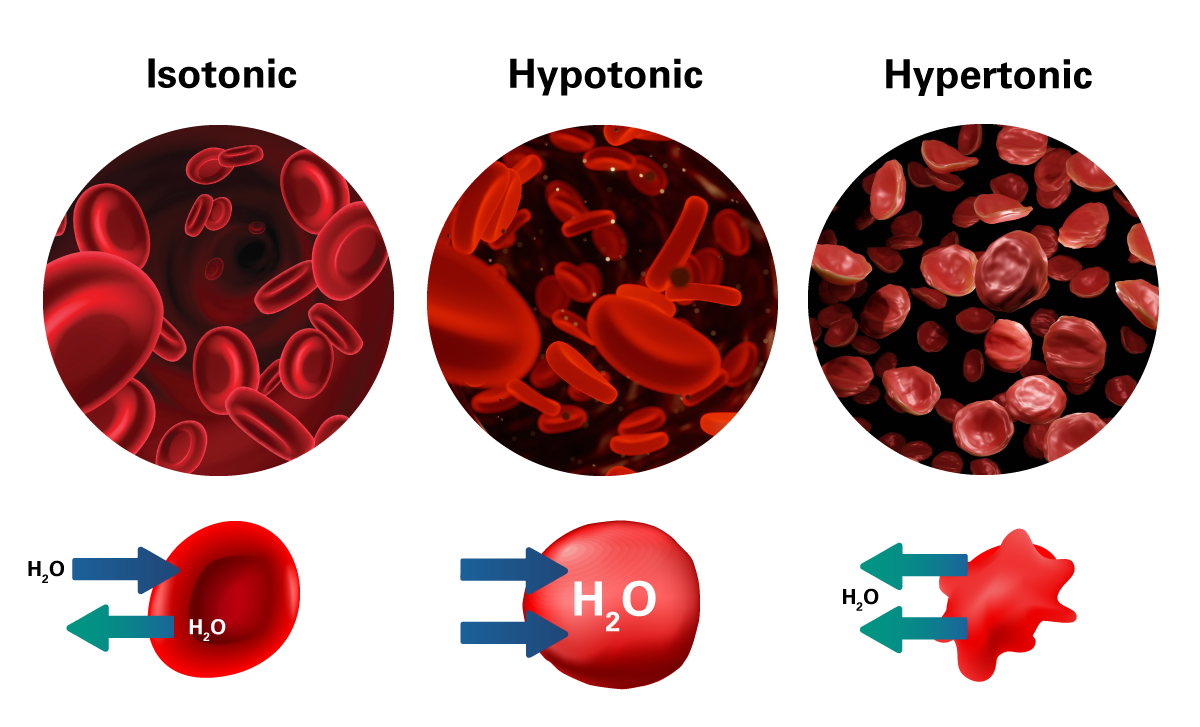 Adapted from Ernstmeyer, K., & Christman, E. (Eds.). (2021). Nursing Skills. https://www.ncbi.nlm.nih.gov/books/NBK593209
Adapted from Ernstmeyer, K., & Christman, E. (Eds.). (2021). Nursing Skills. https://www.ncbi.nlm.nih.gov/books/NBK593209
There are different ways to calculate the flow rates for IV solutions. When the flow needs to be very precise, IV pumps are indicated. The following formula can assist the nurse in accurate calculation:
1. mL/hr (rate for IV infusions on IV pump):
2. gtts/min (rate of IV infusions by gravity):
3.2 Drug Overdose Emergencies
 In the realm of healthcare, drug overdose emergencies are critical situations that demand swift and knowledgeable intervention. These emergencies arise when an individual has ingested or been exposed to an excessive amount of a substance, posing immediate risks to their health and well-being. Recognizing the signs and symptoms of a drug overdose, understanding the specific substances involved, and administering appropriate emergency measures are pivotal aspects of responding effectively to such incidents.
In the realm of healthcare, drug overdose emergencies are critical situations that demand swift and knowledgeable intervention. These emergencies arise when an individual has ingested or been exposed to an excessive amount of a substance, posing immediate risks to their health and well-being. Recognizing the signs and symptoms of a drug overdose, understanding the specific substances involved, and administering appropriate emergency measures are pivotal aspects of responding effectively to such incidents.
Table 1
Drug Overdose Emergencies
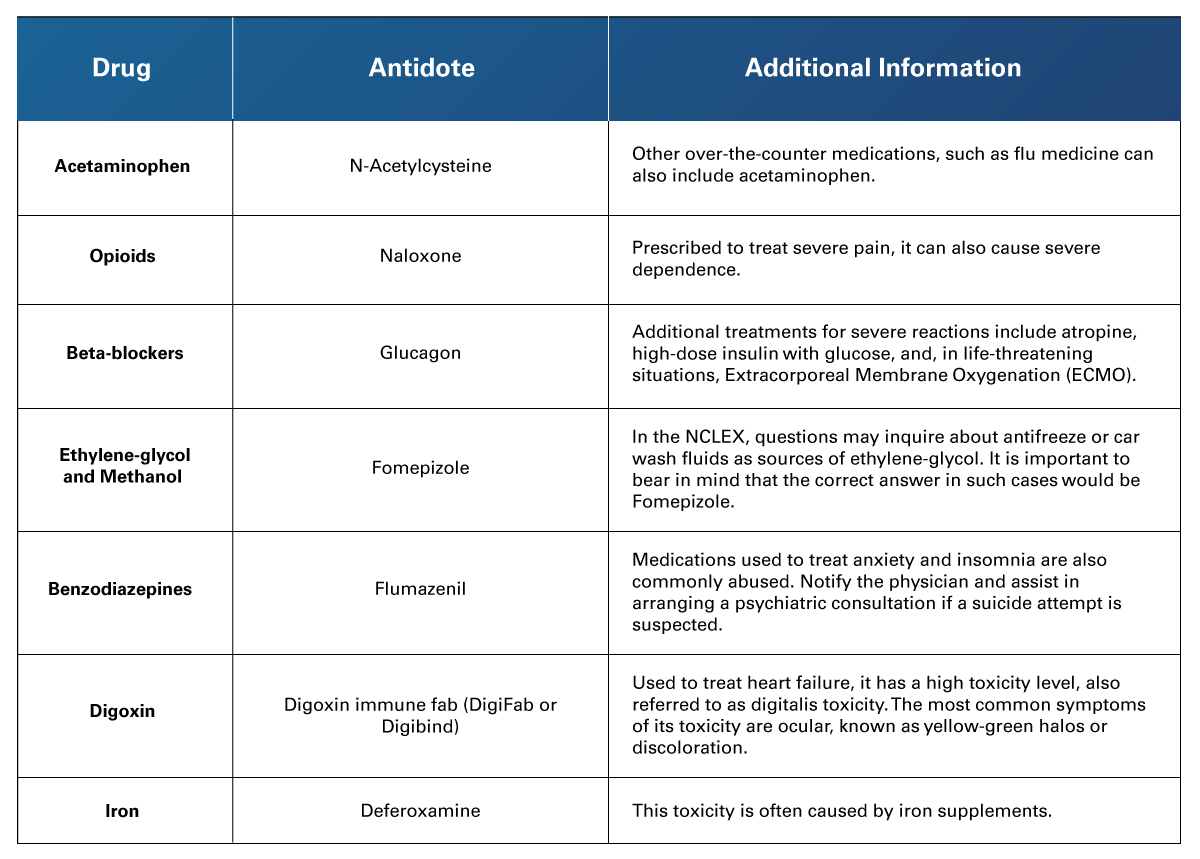 Adapted from Montané, E., & Santesmases, J. (2020). Adverse Drug Reactions. Medicina Clínica (English Edition), 154(5). https://doi.org/10.1016/j.medcle.2019.08.005
Adapted from Montané, E., & Santesmases, J. (2020). Adverse Drug Reactions. Medicina Clínica (English Edition), 154(5). https://doi.org/10.1016/j.medcle.2019.08.005
3.3 Client/Patient Education
 Assessing an ADR in patients/clients should be a routine part of the nursing process. However, this task is largely determined by the patient’s response and their knowledge of their medical history or past ADRs to medications.
Assessing an ADR in patients/clients should be a routine part of the nursing process. However, this task is largely determined by the patient’s response and their knowledge of their medical history or past ADRs to medications.
Here is a list of questions the nurse could ask all clients to assess a possible risk for an ADR and to inform the physician and healthcare team:
- Have you ever taken this medication (clearly name the medication) before without experiencing an adverse reaction?
- If the patient mentions an ADR with a specific drug, ask the following: Did you modify your diet, routine, or anything else around the time you experienced this ADR?
- Did this specific reaction happen immediately or shortly after you started taking the drug?
- Did the ADR stop or go away after you discontinued this medication?
These questions will help you assess the risk of an ADR, report to the healthcare team, and apply a distinctive label to the patient’s charts or documents if an allergy to a specific drug has been previously reported.
It is important to note that while it may be uncommon for a prior reaction or lack of reaction to a specific drug, it does not necessarily indicate that the patient won't or will develop such a reaction again. The physician should assess the risk/benefit in this case. Nevertheless, it remains the responsibility of the nursing staff to furnish the team with all relevant and detailed information.
 This learning experience, in summary, highlights the importance of knowledge in drug safety and administration within nursing practice. Insights into managing adverse drug reactions, understanding the complexities of intravenous therapy, and responding to drug overdoses are invaluable for ensuring patient safety and effective medication management. This expertise is a cornerstone in the nursing field, enhancing patient outcomes and contributing to professional excellence in healthcare.
This learning experience, in summary, highlights the importance of knowledge in drug safety and administration within nursing practice. Insights into managing adverse drug reactions, understanding the complexities of intravenous therapy, and responding to drug overdoses are invaluable for ensuring patient safety and effective medication management. This expertise is a cornerstone in the nursing field, enhancing patient outcomes and contributing to professional excellence in healthcare.
- Ernstmeyer, K., & Christman, E. (Eds.). (2021). Nursing Skills. Chippewa Valley Technical College. https://www.ncbi.nlm.nih.gov/books/NBK593209/
- Frey, N., Bodmer, M., Bircher, A., Jick, S. S., Meier, C. R., & Spoendlin, J. (2019). Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis in association with commonly prescribed drugs in outpatient care other than anti-epileptic drugs and antibiotics: A population-based case-control study. Drug Safety, 42(1), 55-66. https://doi.org/10.1007/s40264-018-0711-x
- Montané, E., & Santesmases, J. (2020). Adverse Drug Reactions. Medicina Clínica (English Edition), 154(5), 178-185. https://doi.org/10.1016/j.medcle.2019.08.005
- World Health Organization. (1972). International Drug Monitoring: The role of National Centers. World Health Organization Technical Report Series, 498, 1–25.
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Videos
- Level Up RN. (2023, April 11). (SJS) Stevens-Johnson Syndrome & (TEN) Toxic Epidermal Necrolysis -Medical-Surgical | @LevelUpRN [Video]. YouTube. https://www.youtube.com/watch?v=Ev-OXDZpb9A
- Rhesus Medicine. (2023, March 28). Understanding Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis (SJS & TEN) [Video]. YouTube. https://www.youtube.com/watch?v=pJzjMSyJUC8
- RegisteredNurseRN. (2023, March 14). IV Fluid Types & Uses Nursing IV Therapy: Isotonic, Hypertonic, Hypotonic Solutions Tonicity NCLEX [Video]. YouTube. https://www.youtube.com/watch?v=NmWBzezefCk
Readings
- U.S. Department of Health and Human Services. (n.d.). Safety Reporting Portal. https://www.safetyreporting.hhs.gov/SRP2/en/Home.aspx?sid=d9d6b1b9-1661-438c-b87c-c9928092e2a3
- Spencer, M. R., White, D. G., & Jackson, G. (2023, May 23). National Hospital Care Survey Demonstration Projects: Mortality Following Nonfatal Opioid Overdose Visits to the Emergency Department. National Health Statistics Reports, 187(May). 1-8. https://dx.doi.org/10.15620/cdc:127054
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.